


The pupillary light reflex arc begins in the retina ( Figure 58.1). The iris dilator fibers contain α-adrenergic sympathetic receptors that respond to changes in sympathetic tonus and changes in the blood level of circulating catecholamines. The size of the pupil is controlled by the activities of two muscles: the circumferential sphincter muscle found in the margin of the iris, innervated by the parasympathetic nervous system: and the iris dilator muscle, running radially from the iris root to the peripheral border of the sphincter. Record these data so that they are easy to read and recall.
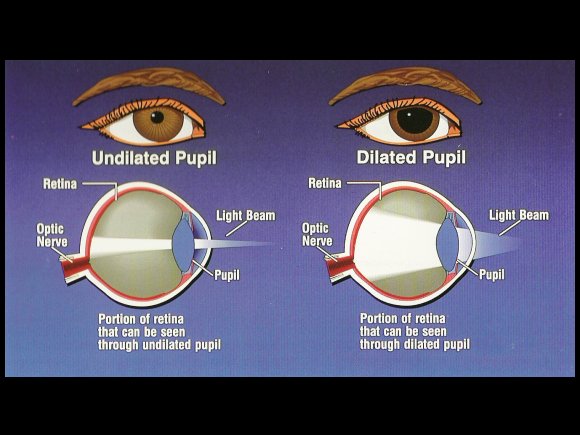
Next, look at the amount of pupillary constriction that occurs when the patient is forced to focus on a near object, such as a thumb held 15 to 20 cm above the eyes. Slowly move the light up to the patient's eye level and check the pupillary response to the bright light on each side several times. To assess pupillary size in a darkened room, illuminate the face from below. For the same reasons, try not to startle or touch patients with your hands or instruments, as psychosensory stimulation induces mydriasis, hippus, and relatively hyperactive pupils. Patients should be encouraged to fixate visually on a distant object, because if they inadvertently look at your nose or the flashlight, the attempt to converge will reflexly evoke miosis, and certain signs may be overlooked (e.g., anisocoria, light-near dissociation, or a subtle Marcus Gunn sign. Because these phenomena are best tested with the pupils in a semidilated state, clinical observations should be made in a dimly lighted room. The examiner first must check the size, shape, equality, and position of the pupils, and their response to a bright light.


 0 kommentar(er)
0 kommentar(er)
